California’s Advancing and Innovating Medi-Cal (CalAIM) seeks to transform the Medi-Cal (California Medicaid) delivery system for more than 14 million Californians, embracing a population health approach that prioritizes prevention and whole-person care and addresses Medi-Cal members’ physical, behavioral, developmental, dental and long-term care needs across the continuum of care.
As a key part of CalAIM, California’s Department of Health Care Services (DHCS) is launching the Population Health Management (PHM) Program in January 2023.1 The PHM Program establishes a statewide, standardized, data-driven approach to ensuring that all Medi-Cal managed care members can access services based on their needs and preferences, ranging from wellness and prevention to care management for the highest-need Medi-Cal members. Together with the PHM Program, DHCS is also launching a statewide “PHM Service” solution in July 2023, which will provide access to current and historical data that is currently disparately available, and support the PHM Program through its statewide standardized Risk Stratification and Segmentation (RSS) algorithm, analytics and other functionalities. The PHM Service is part of a broader, statewide effort to accelerate and expand access to health and social service information among health care entities, government agencies and social services organizations under California’s Data Exchange Framework (DxF).
A critical goal of both the PHM Program and the PHM Service is to address the wide health disparities in the Medi-Cal program for people of color relative to the general population, which have been further exacerbated by the COVID-19 pandemic.
Under PHM, Medi-Cal Managed Care Plans (MCPs) will be working within a common set of baseline expectations while being responsive to individual member needs within local communities. The PHM Program requirements apply specifically to MCPs. However, PHM is a statewide endeavor that interacts with other delivery systems and carved-out services—most notably California’s Specialty Mental Health System, which is county-based—and thus requires meaningful engagement between MCPs and other stakeholders, as well as with members themselves.
Under the new PHM Program, DHCS is setting comprehensive requirements for MCPs within each of the four domains of the PHM Framework (see Figure 1 below):
Figure 1: PHM Framework
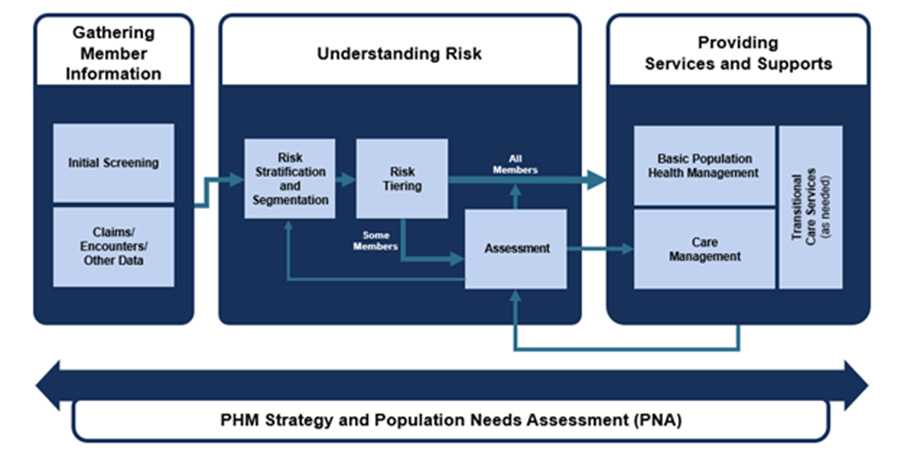
- PHM Strategy and Population Needs Assessment: Foundational to the success of PHM implementation is an overarching data-driven strategy that prioritizes collaboration with community partners. Today in California, MCPs are required to measure health disparities and identify the priority health and social needs of its members through the Population Needs Assessment (PNA). Starting in January 2023, DHCS will revamp the PNA process to include greater community engagement and align with other processes such as the hospitals’ Community Health Needs Assessments and Local Health Departments’ Community Health Improvement Plans. The PNA will also support development of a new annual PHM Strategy, which will detail each component of an MCP’s PHM approach, prioritize strong ties in the community, and incorporate cross-sector strategies to improve health in neighborhoods and communities with poor health outcomes.
- Gathering Member Information: The PHM Program also emphasizes gathering, sharing and assessing timely and accurate individual-level data to identify efficient and effective opportunities for interventions. DHCS will require each MCP to gather and use a wide variety of data to conduct the PHM Program, including data generated within the MCP and externally, including but not limited to provider referrals, member demographics (e.g., race, ethnicity, preferred language), and information from screenings and assessments. When the PHM Service goes online, it will improve and consolidate information available to MCPs from outside the managed care delivery system and provider practices, including members’ health history, needs, and risks leveraging administrative, medical, behavioral, dental, and social service data and other program information from disparate sources. The PHM Service will also use data to support assessment and screening processes.
- Understanding Risk: Prior to the PHM Service going live in July 2023, MCPs are expected to have their own data-driven RSS approaches that consider all information to avoid and reduce bias and prevent exacerbation of health disparities. After the PHM Service is live, it will use collected data to support a statewide standardized RSS algorithm and risk tiering process that will be developed with stakeholder input and a group of national experts. More specifically, the PHM Service will use a risk tiering process which will utilize standardized criteria to place all individuals served by Medi-Cal into a risk tier (i.e., high, medium-rising or low), taking information from all Medi-Cal delivery systems into account. MCPs will be required to use the PHM Service risk tiers as a baseline standard to identify and assess member-level risks and needs and, as needed, connect members to services. MCPs may also use local data sources (i.e., clinical data or ZIP code level social drivers of health data) or real-time data that could supplement these PHM Service outputs for the purpose of identifying additional members for further assessments and services.
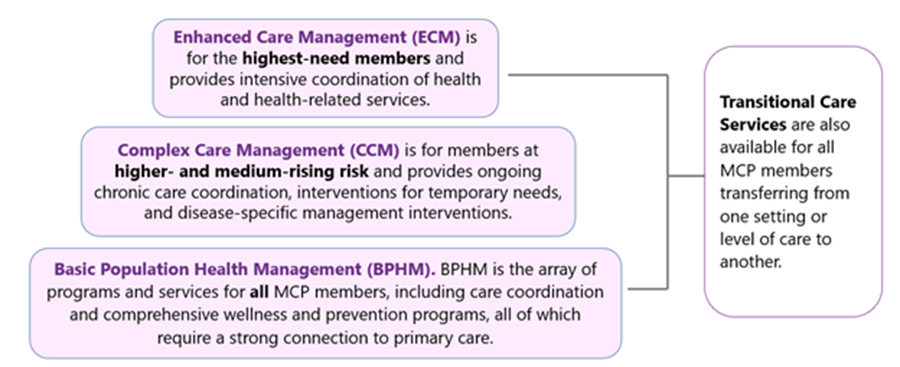
- Providing Services and Supports: One of the main objectives of PHM is to connect MCP members to the right services and supports at the right time and in the right setting depending on their needs and preferences. DHCS will require each MCP to offer supports and programs that members need and want along the continuum of care, which will include Basic Population Health Management (BPHM) for all members; care management programs, including Enhanced Care Management (ECM) or Complex Care Management (CCM) for high-risk and select medium-rising-risk members; and transitional care services for members in care transition (see Figure 2 below). With the PHM Service’s analytics and reporting functionalities, DHCS will have the improved ability to understand population health trends and the efficacy of various PHM interventions as well asstrengthen oversight.
Figure 2: PHM Care Management Continuum
PHM is a journey rather than a destination. Over time, the PHM Program will evolve to support more integration across delivery systems, moving beyond the current requirements for MCPs.
The launch of the PHM Program and deployment of the PHM Service are part of a broader arc of change to improve health outcomes that started with CalAIM and is further articulated in DHCS’ Comprehensive Quality Strategy. Through these collective efforts, California is making important strides in improving whole-person care for Medi-Cal members, reducing health disparities, and making meaningful advances in quality and health outcomes all with the goal of coupling quality and health equity efforts with prevention.