Medicaid’s Critical Role in Addressing the Opioid Crisis
By Patricia Boozang, Senior Managing Director, Manatt Health | Deborah Bachrach, Partner, Manatt Health | Mindy Lipson, Senior Manager, Manatt Health | Adam Striar, Manager, Manatt Health
As the opioid crisis in the United States continues to deepen—with opioid overdoses claiming 42,000 lives in 20161—policymakers, providers, advocates and other stakeholders are seeking out all available resources in an attempt to fight back. However, despite these efforts, the crisis continues to grow. Overdose deaths increased by 28% in 2016 over the previous year.2 Over the past decade, prescription opioid misuse and heroin use have doubled, the national rate of opioid-related emergency department visits nearly doubled,3 and opioid-related inpatient stays increased by almost two-thirds.4
The Medicaid program has proven to be one of the most critical tools in the fight against the opioid crisis by serving as a major source of coverage and payment for substance use disorder (SUD) services across all states. Today, Medicaid covers more than a third of the more than 2 million individuals with an opioid use disorder (OUD) across the country5 and is the predominant source of federal funding for SUD prevention and treatment in many states.6 Leveraging these federal resources, state Medicaid programs have a variety of strategies at their disposal to tailor programs to meet the needs of individuals suffering from OUD in their states, including Medicaid expansion and other, more targeted strategies. This brief highlights Medicaid’s role as a linchpin in the fight against the opioid crisis, in terms of the scale of resources directed by Medicaid toward preventing and treating OUDs and the specific prevention and treatment strategies available to states through the program.
This summary was adapted from two briefs produced by Manatt Health for State Health and Value Strategies, a program supported by the Robert Wood Johnson Foundation. The first, Medicaid: States’ Most Powerful Tool to Combat the Opioid Crisis, was released in July 2016, and the second, Medicaid: The Linchpin in State Strategies to Prevent and Address Opioid Use Disorders, was released in March 2018.
Medicaid Spending on OUD Prevention and Treatment
The federal government uses a number of different channels to support states in responding to the opioid crisis, but Medicaid is by far the most significant and impactful. Medicaid is the largest source of comprehensive coverage for individuals with an OUD, providing access to prevention, treatment and recovery services as well as the full array of physical and behavioral health services to treat co-occurring conditions.7 In federal fiscal year (FFY) 2013, Medicaid spent $9.4 billion in federal and state dollars on comprehensive healthcare services for 636,000 individuals with an OUD.8 Since this time, enrollment of, and spending on, individuals with OUD has undoubtedly increased significantly as a result of Medicaid expansion, and newly eligible adults now represent a majority of Medicaid enrollees with an OUD in many expansion states.9 In comparison, the entire SUD treatment and prevention budget of the Substance Abuse and Mental Health Services Administration (SAMHSA) totaled $2.9 billion in FFY 2017, with approximately $549 million targeted at the opioid epidemic specifically.10
Medicaid Strategies to Combat the Opioid Epidemic
Perhaps the strongest tool that states have at their disposal in the fight against the opioid crisis is Medicaid expansion, which allows states to expand Medicaid coverage to all individuals with incomes up to 138% of the federal poverty level (FPL) while receiving an enhanced federal matching rate for newly eligible adults. This is the most straightforward way for states to extend coverage of comprehensive healthcare services, including a wide range of SUD treatment services, to the greatest number of adults possible—including justice-involved populations at very high risk of addiction. While some have suggested that Medicaid expansion has fueled the opioid epidemic, there is strong evidence to the contrary: Medicaid does not facilitate access to dangerous nonprescription opioids (e.g., heroin and illegally made fentanyl) that account for a large proportion of the recent growth in overdose deaths;11 significant upticks in overdose death rates began prior to expansion; and overdose death rates grew less in counties with the largest gains in Medicaid and other coverage under the Affordable Care Act (ACA) from 2010 to 2015.12
Beyond expansion, state Medicaid programs have a range of additional tools at their disposal to prevent and treat OUDs. These range from modest, but meaningful, strategies for SUD prevention and treatment to more innovative and transformative changes to the way that Medicaid pays for and delivers SUD services. Broadly, these can be accomplished using either state plan authority or Section 1115 waiver authority.
State Plan Strategies
Using the straightforward mechanism of state plan amendments (SPAs), state Medicaid agencies can enhance coverage and benefits, provide robust care management services through the Medicaid Health Home benefit, and leverage Medicaid’s purchasing power to promote best practices by providers and plans. Specifically, states may:
- Implement prior authorization requirements, institute quantity limits and strengthen utilization review criteria for opioid prescriptions;13
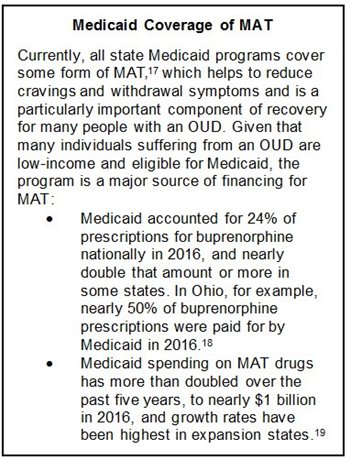
- Improve timely access to medications used in medication-assisted treatment (MAT) by eliminating or modifying prior authorization requirements and reviewing prescription drug policies;14
- Add all forms of naloxone and other evidence-based medications for opioid overdose to their preferred drug lists;15
- Expand Medicaid’s access to and use of the state’s prescription drug monitoring program (PDMP).16
In addition, state Medicaid programs have the opportunity to implement Health Homes to provide robust care management services to individuals with chronic conditions, including individuals with SUDs, while receiving a 90% federal match for the first two years of an individual’s enrollment. States have undertaken a number of initiatives using Health Homes, including providing intensive care management and coordination for individuals with an OUD and provider and workforce education on evidence-based treatment.
Demonstration Waiver Strategies
?width=210&height=185) Section 1115 demonstration waivers give states a pathway to undertake more far-reaching transformations of their SUD delivery systems, draw down additional federal funding to support reform efforts, and hold providers accountable for meeting clinical quality and performance measures related to SUD prevention and treatment.
Section 1115 demonstration waivers give states a pathway to undertake more far-reaching transformations of their SUD delivery systems, draw down additional federal funding to support reform efforts, and hold providers accountable for meeting clinical quality and performance measures related to SUD prevention and treatment.
Federal guidance released in November 2017 urges more states to use this authority to address the opioid crisis specifically.20 A centerpiece of this guidance is encouraging states to apply for waivers of the “IMD exclusion.” This policy has generally prohibited federal financial participation for Medicaid services delivered to individuals residing at institutions for mental diseases (IMDs), and historically has limited the ability of states to provide the full spectrum of care to individuals with SUDs. As of 2013–14, 21 states covered no short- or long-term residential SUD treatment.21 At the time of publication, 10 states22 have received a waiver of the IMD exclusion for SUD services, and 11 states’ applications23 are under review.
Beyond waiving the IMD exclusion, states have used waivers to pursue a number of other innovative strategies aimed at expanding coverage and improving care delivery for individuals with SUDs and other behavioral health conditions.24 Strategies include:
- Expanding Medicaid eligibility to targeted individuals with SUDs. Utah, which has not expanded its Medicaid program under the ACA, extended full Medicaid coverage to childless adults ages 19–64 with incomes less than or equal to 5% of FPL who are chronically homeless or in need of SUD or mental health treatment (including justice-involved populations).25
- Offering enhanced benefits to individuals with SUDs, such as peer recovery supports, SUD-focused targeted case management or nonmedical transportation. For example, California added coverage of recovery services as part of its Drug Medi-Cal Organized Delivery System Pilot Program under its 1115 waiver. These services include outpatient counseling services, recovery monitoring, peer-to-peer assistance and linkages to a variety of social supports.26
- Establishing integrated delivery networks of physical health, behavioral health and social service providers through various payment and delivery system reform initiatives. For example, New Hampshire has established regional integrated delivery networks to improve the continuum of care for Medicaid beneficiaries with SUDs. These networks include primary care providers, SUD providers, community mental health centers, peer health workers, hospitals, community health centers and community-based organizations.
Conclusion
States are grappling day to day with the vast and deadly public health crisis created by the opioid epidemic. As the largest source of comprehensive coverage for individuals with OUD and one of the principal funding sources for the delivery of SUD-related care, Medicaid is the most powerful vehicle available to states to prevent and treat opioid addiction. Through federal flexibility, states can create strategies that meet their specific needs and augment other efforts underway. While the greatest opportunity to address this crisis exists in those states that have elected to expand Medicaid, regardless of expansion status, Medicaid is foundational for states to battle opioid addiction and mortality.
1About Underlying Cause of Death, 1999-2016, CDC Wonder, Centers for Disease Control and Prevention website, U.S. Department of Health and Human Services, https://wonder.cdc.gov/ucd-icd10.html. Accessed March 22, 2018.
2Ibid.
3Saha, T.D., et al., Nonmedical Prescription Opioid Use and DSM-5 Nonmedical Prescription Opioid Use Disorder in the United States, J Clin Psychiatry 77, no. 6, NCBI website, https://www.ncbi.nlm.nih.gov/pubmed/27337416. Published June 2016. Accessed March 22, 2018.
4Weiss, A.J., et al., Opioid-Related Inpatient Stays and Emergency Department Visits by State, 2009-2014, Statistical Brief #219, Healthcare Cost and Utilization Project website, Agency for Healthcare Research and Quality, https://www.hcup-us.ahrq.gov/reports/statbriefs/sb219-Opioid-Hospital-Stays-ED-Visits-by-State.jsp. Published December 2016. Updated January 2017. Accessed March 22, 2018.
5Medicaid’s Role in Addressing the Opioid Epidemic, Kaiser Family Foundation website, https://www.kff.org/infographic/medicaids-role-in-addressing-opioid-epidemic/. Published February 27, 2018. Accessed March 22, 2018.
6Grady, A. et al., Medicaid: The Linchpin in State Strategies to Prevent and Address Opioid Use Disorders, State Health and Value Strategies, https://www.shvs.org/wp-content/uploads/2018/03/SHVS_Medicaid-Opioids_Final.pdf. Published March 2018. Accessed March 22, 2018.
7Medicaid’s Role in Addressing the Opioid Epidemic, Kaiser Family Foundation website, https://www.kff.org/infographic/medicaids-role-in-addressing-opioid-epidemic/. Published February 27, 2018. Accessed March 22, 2018.
8Young, K. and Zur, J., Medicaid and the Opioid Epidemic: Enrollment, Spending, and the Implications of Proposed Policy Changes, Kaiser Family Foundation website, http://files.kff.org/ attachment/Issue-Brief-Medicaid-and-the-Opioid-Epidemic-Enrollment-Spending-and-the-Implications-of-Proposed-Policy-Changes. Published July 2017. Accessed March 22, 2018.
9Grady, A. et al., Medicaid: The Linchpin in State Strategies to Prevent and Address Opioid Use Disorders, State Health and Value Strategies, https://www.shvs.org/wp-content/uploads/2018/03/SHVS_Medicaid-Opioids_Final.pdf. Published March 2018. Accessed March 22, 2018.
10Fiscal Year 2018: Justification of Estimates for Appropriations Committees, Manatt analysis of amounts in Substance Abuse and Mental Health Services Administration, U.S. Department of Health and Human Services, SAMHSA website, https://www.samhsa.gov/sites/default/files/samhsa-fy-2018-congressional-justification.pdf. Accessed March 22, 2018.
11Opioid Data Analysis, Centers for Disease Control and Prevention, U.S. Department of Health and Human Services website, https://www.cdc.gov/drugoverdose/data/analysis.html. Accessed March 22, 2018.
12Goodman-Bacon, A. and Sandoe, E., Did Medicaid Expansion Cause The Opioid Epidemic? There’s Little Evidence That It Did, Health Affairs Blog, https://www.healthaffairs.org/do/10.1377/hblog20170823.061640/full/. Published August 23, 2017. Accessed March 22, 2018.
13Wachino, Vikki. Best Practices for Addressing Prescription Opioid Overdoses, Misuse and Addiction. Baltimore: Center for Medicaid and CHIP Services, 2016. Accessed March 22, 2018. Mercer. State Medicaid Interventions for Preventing Prescription Drug Abuse and Overdose. Phoenix: Mercer, 2014. Accessed March 22, 2018. http://medicaiddirectors.org/wp-content/uploads/2015/07/namd_rx_abuse_report_october_2014.pdf; Mann, Cindy, Thomas Frieden, Pamela S. Hyde, Nora D. Volkow, and George F. Koob. Medication Assisted Treatment for Substance Use Disorders. Baltimore: Centers for Medicare and Medicaid Services, 2014. Accessed March 22, 2018. https://www.medicaid.gov/federal-policy-guidance/downloads/cib-07-11-2014.pdf.
14Substance Abuse and Mental Health Services Administration. Medicaid Coverage and Financing of Medications Used to Treat Alcohol and Opioid Use Disorders. Rockville: Substance Abuse and Mental Health Services Administration, 2014. Accessed March 22, 2018. Wachino, Vikki. Best Practices for Addressing Prescription Opioid Overdoses, Misuse and Addiction. Baltimore: Center for Medicaid and CHIP Services, 2016. Accessed March 22, 2018. Mercer. State Medicaid Interventions for Preventing Prescription Drug Abuse and Overdose: A Report for the National Association of Medicaid Directors. Phoenix: Mercer, 2014. Accessed March 22, 2018. http://medicaiddirectors.org/wp-content/uploads/2015/07/namd_rx_abuse_report_october_2014.pdf.
15Wachino, Vikki. Best Practices for Addressing Prescription Opioid Overdoses, Misuse and Addiction. Baltimore: Center for Medicaid and CHIP Services, 2016. Accessed March 22, 2018. Mann, Cindy, Thomas Frieden, Pamela S. Hyde, Nora D. Volkow, and George F. Koob. Medication Assisted Treatment for Substance Use Disorders. Baltimore: Centers for Medicare and Medicaid Services, 2014. Accessed March 22, 2018. https://www.medicaid.gov/federal-policy-guidance/downloads/cib-07-11-2014.pdf.
16Wachino, Vikki. Best Practices for Addressing Prescription Opioid Overdoses, Misuse and Addiction. Baltimore: Center for Medicaid and CHIP Services, 2016. Accessed March 22, 2018. Mercer. State Medicaid Interventions for Preventing Prescription Drug Abuse and Overdose. Phoenix: Mercer, 2014. Accessed March 22, 2018. http://medicaiddirectors.org/wp-content/uploads/2015/07/namd_rx_abuse_report_october_2014.pdf; Alexander, G. Caleb, Shannon Frattaroli, and Andrea C. Gielen. The Prescription Opioid Epidemic: An Evidence-Based Approach. Baltimore: Johns Hopkins Bloomberg School of Public Health, 2015. Accessed March 22, 2018. https://www.jhsph.edu/research/centers-and-institutes/center-for-drug-safety-and-effectiveness/research/prescription-opioids/JHSPH_OPIOID_EPIDEMIC_REPORT.pdf.
17Use of Opioid Recovery Medications: Recent Evidence on State Level Buprenorphine Use and Payment Types, IMS Institute for Healthcare Informatics website https://www.iqvia.com/-/media/iqvia/pdfs/institute-reports/use-of-opioid-recovery-medications.pdf. Published September 2016. Accessed March 22, 2018 Spending reflects amounts paid to pharmacies; the net cost to Medicaid is lower after accounting for rebates from manufacturers, but rebate amounts are not publicly available for individual drug products.
18Clemans-Cope, L., Epstein, M., and Kenney, G.M., Rapid Growth in Medicaid Spending on Medications to Treat Opioid Use Disorder and Overdose, Urban Institute website, https://www.urban.org/sites/default/files/publication/91521/2001386-rapid-growth-in-medicaid-spending-on-medications-to-treat-opioid-use-disorder-and-overdose_2.pdf. Published June 2017. Accessed March 22, 2018.
19Gifford, K., Ellis, E., Coulter Edwards, B., and Lashbrook, A., Health Management Associates; and Hinton, E., Antonisse, L., Valentine, A., and Rudowitz, R., Kaiser Family Foundation, Medicaid Moving Ahead in Uncertain Times: Results from a 50-State Medicaid Budget Survey for State Fiscal Years 2017 and 2018, Kaiser Family Foundation website, https://www.kff.org/medicaid/report/medicaid-moving-ahead-in-uncertain-times-results-from-a-50-state-medicaid-budget-survey-for-state-fiscal-years-2017-and-2018/.
20Strategies to Address the Opioid Epidemic, SMD 17-003, U.S. Department of Health and Human Services, Centers for Medicare & Medicaid Services website, https://www.medicaid.gov/federal-policy-guidance/downloads/smd17003.pdf. Dated November 1, 2017. Accessed March 22, 2018.
21Grogan, C.M., Andrews, C., Abraham, A., Humphreys, K., Pollack, H.A., Tran Smith, B., and Friedmann, P.D., Survey Highlights Differences in Medicaid Coverage for Substance Use Treatment and Opioid Use Disorder Medications, Health Affairs website, Health Affairs 35, no. 12, https://www.healthaffairs.org/doi/abs/10.1377/hlthaff.2016.0623. Published November 1, 2017. Accessed March 22, 2018.
22California, Indiana, Kentucky, Louisiana, Maryland, Massachusetts, New Jersey, Utah, Virginia, and West Virginia have obtained a waiver of the IMD exclusion for SUD services.
23Alaska, Arizona, Illinois, Michigan, Minnesota, New Mexico, North Carolina, Washington, and Wisconsin have pending applications to waive the IMD exclusion; this list also includes Massachusetts, which is seeking to broaden the scope of its IMD waiver, and Vermont, which has obtained a waiver of the IMD exclusion for mental health services, but not for SUD.
24Information based on Manatt analysis of Section 1115 waiver documents available on Medicaid.gov.
25Since Utah has not expanded its Medicaid program under the ACA, it is unable to obtain the ACA’s enhanced federal medical assistance percentage (FMAP) for this population; instead it receives its regular FMAP.
26While states may also use State Plan authority to add new SUD benefits, many states have chosen to expand the benefits they offer to Medicaid enrollees with SUDs through 1115 waivers.
27Goodman-Bacon, A. and Sandoe, E., Did Medicaid Expansion Cause The Opioid Epidemic? There’s Little Evidence That It Did, Health Affairs Blog, https://www.healthaffairs.org/do/10.1377/hblog20170823.061640/full/. Published August 23, 2017. Accessed March 22, 2018.
back to top
New Webinar: America's Multidimensional Opioid Crisis
As the crisis of addiction accelerates, experts project that opioids could kill nearly half a million Americans over the next decade. Already, close to 100 people a day die from opioids.1
How did the crisis begin? Where are we now? And what can we do going forward? In a new webinar for Bloomberg BNA, Manatt reveals the answers, examining the opioid crisis from the diverse viewpoints of its affected stakeholders, including victims and their families, first responders and law enforcement agencies, pharmaceutical manufacturers, states and cities, and public and private payers. Topics covered include:
- The genesis and drivers of the opioid crisis from multiple vantage points
- Short- and long-term strategies that cities, states and the federal government are using to address the crisis through litigation, enforcement and regulation
- The actions both the public and private sectors are taking to combat the crisis
- Opioid-related civil and criminal cases brought by cities and counties, state attorneys general, and the Department of Justice
- The ways False Claims Act theories used in other pharma cases may be applied in opioid cases moving forward
- The innovative solutions emerging across the full range of stakeholders, including pharmaceutical companies, government payer programs and private insurers
- The next steps for cities and states in terms of policies, education, community engagement, treatment options and more
- A look ahead at what the future holds for law enforcement, from the increasing use of data analytics to new theories of liability
- Next steps to change laws, regulations and treatment protocols to ameliorate the crisis
Presenters:
Joel Ario, Managing Director, Manatt Health
Jocelyn Guyer, Managing Director, Manatt Health
Richard Hartunian, Partner, Corporate Investigations and White Collar Defense
Jacqueline Wolff, Partner, Co-chair, Corporate Investigations and White Collar Defense, and Co-chair, False Claims Act Practice
1STAT Forecast, June 27, 2017
back to top