Academic Health System Cancer Programs: Eight Fundamental Elements to Reassess in the Current Environment
Patients and referring physicians look to Academic Health Systems (AHSs) for access to increasingly complex novel and breakthrough therapies, clinical trials and highly specialized expertise in advanced diagnostics and treatment as the field of cancer care rapidly changes. Federal level research funding cuts, reductions in reimbursement and other market forces present challenges for cancer program operations and financial performance.
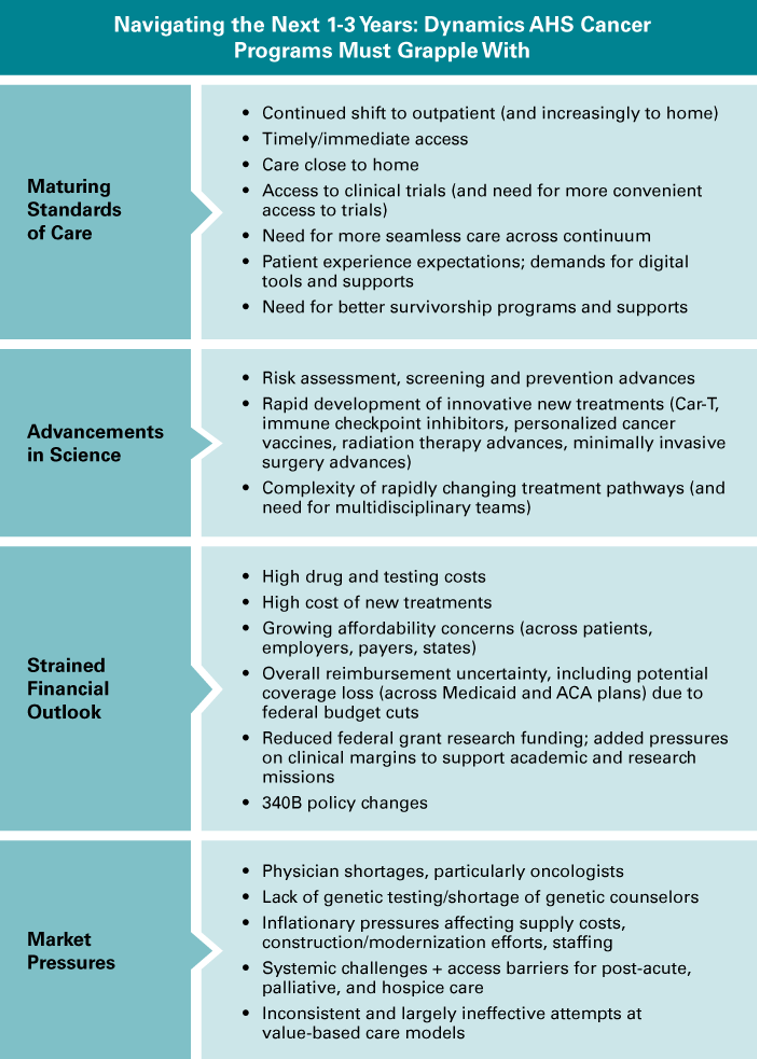
Cancer services and service lines are the most complex for AHSs to organize and manage, given the many specialties and services involved and the complex interrelationships between the clinical, teaching and research missions. There is great variation in how these programs are organized and funded but demands for operational excellence are universal.
Eight Cancer Program Fundamentals to Reassess
A thoughtful and structured review of cancer program infrastructure and strategies across the following eight program elements will help AHS leaders proactively address gaps and vulnerabilities and foster organizational alignment around priorities heading into challenging times:
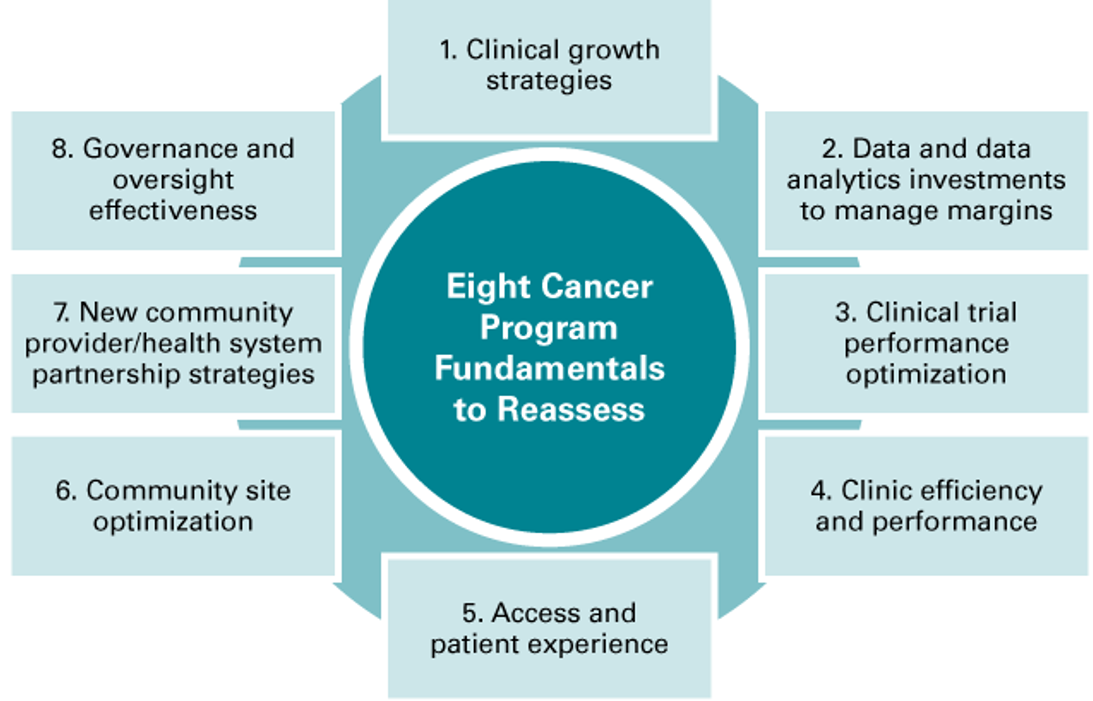
1. Clinical growth strategies: Strong disease-site oriented programs comprised of clinical professionals and care teams with specialized expertise and linkages to basic and translational research, supported by an appropriate multidisciplinary care platform are “table stakes” for AHS cancer programs. Regular monitoring of patient migration patterns at a granular level and proactive communication should be used to elevate trends, threats, and clinical investment needs to executive leaders across the health system and school of medicine. As a proactive strategy, programs should implement ongoing outreach to referring physicians, promoting their disease-site and clinical trials expertise and ease of access.
2. Data and data analytics investments to manage margins: Downward pressure on revenue and rapidly growing costs are compressing margins. Actionable data has never been at a higher premium.
- Financial – data should include contribution margin by service type, disease site and location for multi-site systems.
- Patient level – Patient specific data in real time tracking utilization of services (i.e. admissions, LOS, ICU days and ED visits) empowers timely proactive intervention. For example, can patients be discharged with support at home or in a hospital-at-home for symptom management to reduce the length of stay? Can early palliative care be expanded?
Proactive management and access to data and analytic resources is essential for managing patients and cancer program financial performance.
3. Clinical trial performance optimization: With reduced federal grant funding, especially for investigator-initiated trials, it has become more important for organizations to optimize their clinical trial portfolio and performance. Staffing, workflow and financial performance have not been as rigorously managed as clinical operations, where financial pressures have existed much longer, and the multiunit structures of AHSs complicate improvement efforts. Trial portfolios are determined in the disease areas and cancer sub-specialties, often causing variation in program strength. Additionally, pharmaceutical companies struggle with accrual to cancer trials, especially in the U.S., and they want relationships with high-performing cancer clinical trial programs.
AHSs should assess the performance and efficiency of their cancer clinical trials program which will require a review of the essential functions that span: research administration, a clinical trials office, a cancer clinical trials office, cancer specialty clinical divisions/departments, the faculty practice plan/medical group, and the cancer service line. A cancer clinical trial plan should specifically address scientific, patient accrual and financial performance.
4. Clinic efficiency and performance: A challenge common to every academic health system/medical school partnership is the allocation of faculty time and its alignment with funding sources. With increasing financial pressures—and in particular as financial dependence on clinical income intensifies—organizations should work to ensure that clinical productivity targets are well-communicated and realized. Some strategies to consider include:
- Physician Clinic Templates – reviewing physician clinic templates to ensure they are optimized and aligned with access, financial, teaching, and research goals;
- Advanced Practice Providers (APPs) – standardizing and expanding the role of APPs in the clinic to ensure they work to the top of their license across all disease site areas;
- Oncology Hospitalists – considering an oncology hospitalist model to reduce inpatient service requirements so there is more time for physicians in the clinic;
- Support staff – assessing the staffing of support personnel (e.g. Medical Assistants) to support an efficient clinic operation;
- Clinical trial support staff – developing plans to reduce turnover of clinical research support staff so that there is less burden on physicians to be engaged in clinical trials.
5. Access and patient experience: A celebrated implication of success in the treatment of cancer is the fact that many patients will now have a long-term relationship with their cancer provider and program. Patients have choices and the market values rapid access for new patient appointments, symptom management, and home-based treatment. Programs need to prioritize the patient experience from the initial call through treatment and into survivorship. Patients value timely access, a live person answering calls, staff to help with resolution of financial challenges, tight coordination of care, effective provider communication, symptom management in the community or at home, and decentralized clinical trials that make participation less of a burden. Programs need to be organized and resourced to meet these needs.
6. Community site optimization: Patients prefer care close to home and deserve patient-centered care at all locations. Academic cancer programs are rapidly expanding their community location options; the standard of care in community-based locations should, to the extent possible, match that in the tertiary setting. Strategies include deployment of surgical specialists and disease-site medical oncologists for the more common cancers to community locations with protocols for seamless handoffs to the AMC and offering the full complement of wrap-around services to patients either in the community setting and/or virtually.
7. New community provider/health system partnership strategies: The value exchange between academic centers and community partners has not always been crisply articulated or realized. Local access to cancer services benefits not only patients but local providers. Solidified referral patterns and increased accrual to trials are among the value propositions for the academic partner. Steps should be taken not only to launch new partnerships with clearer expectations, but also to revisit existing relationships to ensure that the expected value is being delivered. Some key considerations include:
- Each party having clear and realistic expectations;
- Medical and administrative leaders from each organization with partnership-building skills and mutual familiarity with the different settings;
- Both organizations having physicians who are committed to the partnership.
8. Governance and oversight effectiveness: In uncertain times, effective governance and oversight is essential. Organizational models vary—some operate as a clinical service line and others as a federation of clinical departments. Either approach must coordinate multiple specialties (including oncology, surgery, pathology, imaging, social work, nutrition, palliative care, etc.), as well as other organizational functions including nursing, finance, IT, marketing and communications, development, etc. Typically, there is dyad leadership with a full-time Vice President (VP) or Senior VP level administrative director and a medical director whose time commitment reflects the size of the program.As described in further detail in our Manatt Health on service lines in AHSs, four key features of effective service line governance to be assessed are noted below. To what extent does your program have:
- A governance structure (i.e. with an executive council) that will work with and support the service line leaders;
- A highly engaged administrative and clinical leadership dyad;
- Clarity of roles between service lines and clinical departments;
- Accountability for key service line functions that makes clear who is ultimately responsible and makes the final decisions.
With the importance of cancer programs and the external factors at play, AHS leaders should assess these eight strategic priorities and take steps to ensure that these vital programs remain strong into the future.
The Structure of Academic Cancer Service Lines: Results of an Association of American Cancer Institutes survey. JCO 42, e13566-e13566(2024). DOI:.
Fracasso P, Simone N, Si Lim S, Reckamp K, Sosa JA, Lieu C, Lee C, Werner T, Ly Q, Vose J, White J, Honeycutt H, Shaw K, Cameron K, O’Brien D, Wilke L. Benchmarking the Current Landscape: Insights from an Association of American Cancer Institutes Survey on Academic Cancer Service Lines, JOP Manuscript in press 2025.
O’Brien D, Sher R, Morin A. Achieving a High Performance, Diverse Accrual, Clinical Trial Program in an Academic Health System, Manatt Health, May 2024.
O’Brien D. Six Actions for Academic Health System Leadership to Achieve a High-Performing Clinical Trials Program. Manatt Health White Paper. August 21, 2025.
Ingraham M, O’Brien D, Pawlak B, Strategies for Meeting Patient Expectations and Improving Patient Experience During Cancer Treatment, Manatt Health, October 2024.
Kaluzny, A., O’Brien, D., Managing Disruptive Change in Healthcare: Lessons from a Public-Private Partnership to Advance Cancer Care and Research, Oxford University Press, New York, (August 2015).
Lorbiecki S, Cetin Z, Enders T, Leary T Frohlich J. Service Line Development in Academic Health Systems. Manatt Health, January 2022 .
