Nutrition as Medicine: California’s Evolving Efforts within the Medi-Cal Program
The Big Picture
For Americans with diet sensitive conditions, a strong evidence base indicates that “Medically Supportive Food and Nutrition (MSF&N) Services”—which include a spectrum of nutritional interventions—can help avoid unnecessary and costly medical care. Accordingly, federal and state government, and many private payers, are increasingly supporting reimbursement for these services as part of efforts to improve health. Below, we explore an example within this broader trend, namely California’s recent experience integrating MSF&N services within its Medi-Cal program. Driven by input from communities and experts, Medi-Cal’s MSF&N services have evolved to an increasingly standardized offering designed to meet program quality and outcome goals.
The evolution of “Nutrition as Medicine” within California’s Medi-Cal program
California originally launched its Medically Tailored Meals/Medically Supportive Foods (“MTM/MSF”) service in January 2022 as one of its authorized by CMS under . California’s vision for all 14 Community Supports is to allow Medi-Cal managed care plans the option to provide alternatives to traditional medical care that are more cost effective and are medically appropriate for a Medi-Cal member. California’s Community Supports broke new policy ground by using the “in lieu of services” Medicaid authority to establish that services addressing social drivers of health can stand in for covered medical services (at the option of the member) by preventing the need for downstream medical care. Between 2022 and 2024, CMS formalized this authority through a .
California’s original definition of the MTM/MSF service established that the service could include “Medically Tailored Meals” (defined as meals “tailored to the medical needs of the member by a Registered Dietitian or other certified nutrition professional, reflecting appropriate dietary therapies based on evidence-based nutritional practice guidelines”) or “Medically-supportive food and nutrition services” (defined as including medically supportive groceries, healthy food vouchers and food pharmacies). Managed care plans have the discretion to define the level and combination of interventions that they consider medically appropriate and cost effective.
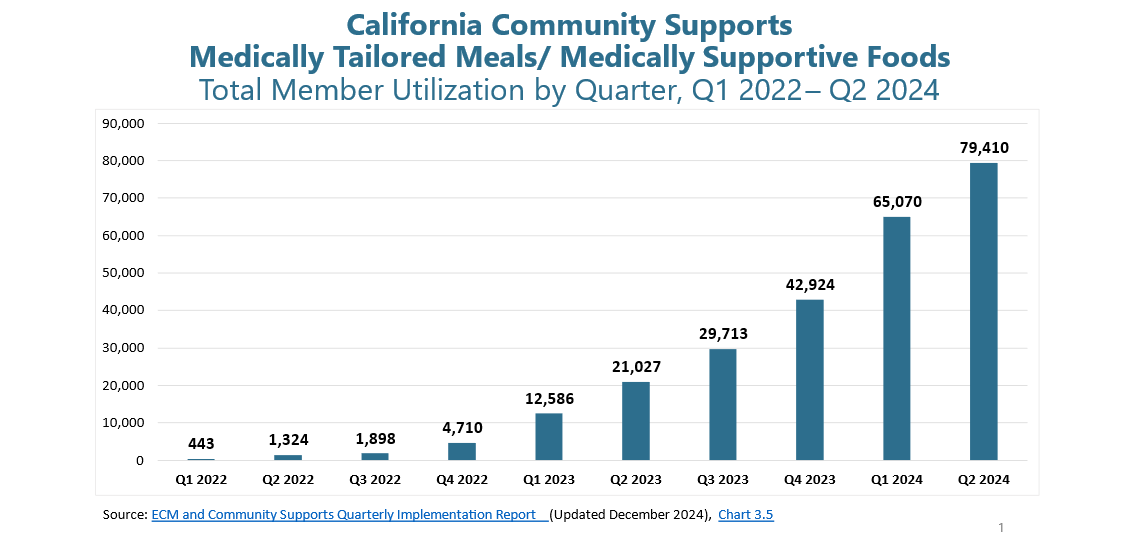
In the first two years of the program (2022–2024), the state heard widespread calls from plans, providers, CBOs and others for further standardization of both the 14 Community Supports to improve fidelity to program intent and equitable access to the services. In 2023, DHCS published an “Action Plan” with steps to standardize the services. During the same period, utilization of the , and by early 2024, was the most utilized Community Support service, making it a high priority for service definition for improved standardization.
In mid-2024, California announced its intention to make improvements to the original MTM/MSF policy. A public comment period brought in nearly 50 letters on MTM/MSF, including detailed input from the field of “Food is Medicine” providers as well as managed care plans and counties. In response to this detailed feedback, :
- Streamlined eligibility criteria. The original definition allowed disparate interpretations of eligibility. In the updated service definition, California has refocused eligibility on whether the Member has a nutrition-sensitive health condition (e.g. cardiovascular disorders, diabetes, human immunodeficiency virus, high-risk perinatal conditions) appropriate for MTM/MSF services according to the evidence base—whether or not the Member may also be experiencing food insecurity. An expanded and refined list of health conditions is given, while acknowledging that it may not be exhaustive.
- Improved definitions of the sub-services. The original definition did not distinguish between “medically tailored” and “medically supportive” services and created confusion about the level of “tailoring” required. Drawing on detailed feedback from the Food is Medicine Coalition and , the updates clarify that MSF services, including medically supportive groceries or produce prescriptions, are intended to be supplemental to the Member’s diet, whereas “medically tailored” interventions must be “tailored” to the targeted condition and be provided in specified quantities that constitute two thirds of the Member’s food for a period of time, in order to have the intended impact on health outcomes.
- Roles of Registered Dietician Nutritionists (RDNs) or other appropriate clinicians. The updates clarify that medically tailored services must include an individual nutrition assessment conducted or overseen by an RDN to inform the development of a nutritional plan in connection with appropriate, medically tailored services for the Member’s diet-sensitive health condition. Additionally, the medically tailored meal or food packages themselves must be tailored to the condition(s) by an RDN or other appropriate clinician based on established, evidence-based nutrition guidelines for that targeted nutrition-sensitive condition. The design or selection of foods or food options in MSF services must be overseen and signed off on by an RDN or another appropriate clinician but do not require an individual assessment by an RDN.
- Provider and Meal/Food Package Oversight: As the MTM/MSF sector grows, increased managed care plan oversight of providers and the food itself is essential. In the service definition update, DHCS outlines requirements on managed care plans for reviewing the quality and safety of MTM/MSF interventions. These requirements apply for MTM/MSF services delivered by both current and prospective MTM/MSF Community Supports Providers to ensure members receive high quality meals/food tailored to their clinical needs.
Looking Ahead for MSF&N Services
Having listened to feedback from providers of MSF&N services, California’s updated policies reflect current thinking on the evidence base and interventions. Notably, the Food is Medicine Coalition has launched a for providers of MSF&N services, with modules that include the integration of RDNs, management of referrals and intake and nutrition education. Additionally, a coalition of Food is Medicine experts, together with the Gravity Project, recently submitted to CMS a set of for these services. These and other efforts to increase the specificity of standard will continue to ensure as strong a connection as possible between the interventions and demonstrable health outcomes in the population.
The policy road ahead for Medicaid to support MSF&N services is unclear at the national level. CMS last week , and . That said, the Trump Administration’s “Make America Healthy Again” agenda may align with and expand MSF&N services. A February to “redirect our national focus, in the public and private sectors, toward understanding and drastically lowering chronic disease rates and ending childhood chronic disease… including by studying contributing factors such as the American diet.” Our hope is that as more states further invest in MSF&N services and, like California, refine services with a focus on quality and improved health outcomes of individuals, MSF&N will continue to be an example of common policy ground to promote improved health of Americans.
Sautter, J. M., Henstenburg, J. A., Crafford, A. G., Rowe-Nicholls, I., Diaz, V. S., Bartholomew, K. A., Evans, J. S., Johnson, M. R., Zhou, J., & Ajeya, D. (2024).
Berkowitz, S. A., Delahanty, L. M., Terranova, J., Steiner, B., Ruazol, M. P., Singh, R., Shahid, N. N., & Wexler, D. J. (2019).
