The Rural Hospital Telehealth Playbook: Case Studies and Strategies
Below is an excerpt from a recent providing rural hospital leaders with a roadmap for leveraging telehealth partnerships. The was written by Medical University of South Carolina and Manatt Health. Click to read the full playbook, including case studies and on-the-ground strategies.
Rural hospitals provide essential care and anchor local economies, supporting 1 in 12 jobs and nearly $220 billion in economic activity in rural communities. Many of these hospitals are facing significant threats to their sustainability, driven by mounting financial strain, workforce shortages, and aging and limited infrastructure. As hospitals struggle with reductions in service capacity and the risk of closures, vulnerable rural communities are faced with decreased access to vital care and the destabilization of their local economies. Against this backdrop, the Medical University of South Carolina (MUSC) has how telehealth partnerships can both stabilize rural hospitals today and help create a more sustainable model of rural care for the future.
In South Carolina, where over 27% of residents live in rural areas and close to 30% of rural hospitals are at risk of closure, MUSC has nearly two decades of experience helping rural hospitals establish telehealth programs that strengthen their sustainability. MUSC has partnered with more than 40 hospitals, varying in size, resources, and geography, to establish telehealth programs from telestroke and tele-ICU to virtual nursing and virtual behavioral health. Across MUSC’s rural hospital partnerships, telehealth has driven higher admission volumes, reduced transfers and readmissions, supported care for more complex patients, and delivered measurable quality improvements. This Rural Hospital Telehealth Playbook draws on MUSC’s expertise to support rural hospital leaders interested in using telehealth partnerships strategically as a core component of their institutions’ financial, operational, and clinical strategy.
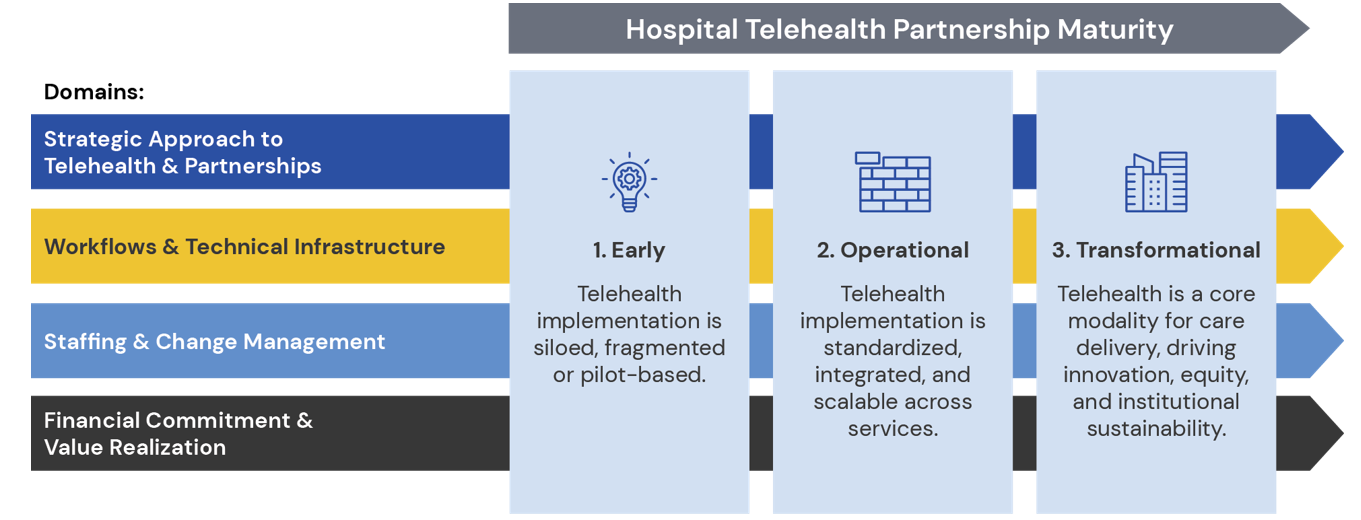
introduces a telehealth partnership maturity model to serve as a roadmap for rural hospitals to strengthen their telehealth strategy. It provides a practical framework to help rural hospitals assess the maturity of their telehealth partnerships and chart a path toward more transformational use of telehealth. The model outlines three levels of telehealth partnership maturity for hospitals—early, operational, and transformational—across four domains of key implementation considerations.
Hospital Telehealth Partnership Maturity Model
For each domain, the provides useful tactics that MUSC and its partners have used to strengthen their telehealth operations, and which rural leaders can adapt to their local context. Direct examples from the MUSC Center for Telehealth and MUSC rural hospitals are woven throughout the Playbook, including an illustrative case study on MUSC Health Black River Medical Center, a newly built rural hospital envisioned as a “rural hospital of the future,” which fully integrates telehealth into daily operations and multiple levels of service delivery.
Taken together, the Playbook is meant to serve as a concrete resource for rural hospital leadership focused on using telehealth to build a more sustainable way to deliver care, remain operational, and continue to serve their local communities.
Click to download the full playbook.
MUSC authors and contributors: Emily Warr, MSN, RN; James McElligott, MD, MSCR; Allen Abernethy, MSRT(R), RRA; Dee Ford, MD, MSCR; Jay Hinesley, MHA, FACHE; Matthew Littlejohn, MHA, FACHE; Yotam Papo, MD, MPH; Matt Severance, MBA, MHA, FACHE; Dunc Williams, MHA, PhD
American Hospital Association. (2022). Rural hospital closures threaten access: Report.
Medical University of South Carolina. (2023). Rural health access: Progress notes, Spring 2023.
Center for Healthcare Quality & Payment Reform. (2025). Rural hospitals at risk of closing.
