Understanding the New CMMI GUIDE Model
The CMS Center for Medicare and Medicaid Innovation (CMMI) is launching a new Alternative Payment Model (APM) focused on Dementia Care: The GUIDE model. It will launch in July 2024 and run for eight years. More details will be forthcoming in the request for applications (RFAs) to be published this fall, which will open the application period for provider organizations. The Model has three primary goals:
- Improving quality of life for people living with dementia
- Improving services, supports and assistance for caregivers of people with dementia
- Delaying nursing home care and enabling more people to live at home through the end of life
In addition, CMMI has included a focus on health equity with this model, including payment adjustments and a required health equity plan by model participants.
Overview of Model
Under the GUIDE model, there will be standardized care delivery requirements, data reporting requirements and a new Medicare payment structure.
Care Delivery Requirements: A comprehensive set of care delivery requirements including structure of team will be included in the GUIDE model, including:
- Care management expectations: comprehensive assessment, care plan, 24/7 access for beneficiaries, medication management, coordination and referral support
- A requirement for support and care to be provided by an interdisciplinary team that includes at a minimum a dementia proficient clinician and a trained care navigator
- A requirement for Caregiver Support including educational classes and respite services
Data Reporting Requirements: The GUIDE model will include requirements for providers to collect and/or report on data such as high-risk medication use, beneficiary quality of life and caregiver burden; care delivery data; beneficiary and caregiver assessment data; and sociodemographic and health-related social needs data.
Medicare Payment Structure: Payment includes a monthly payment with adjustments as well as additional payment for respite services to allow relief for caregivers.
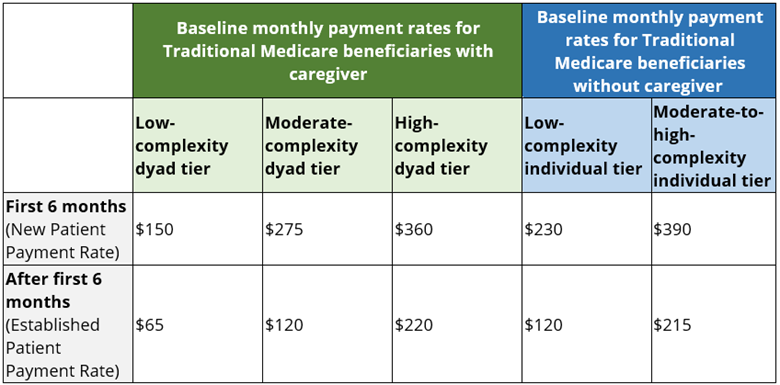
Monthly Payment: Payment for the GUIDE model will include a per beneficiary per month payment for aligned Traditional Medicare lives using claims for a Dementia Care Monthly Payment. It will be adjusted based on severity of illness, presence of caregiver and length of program enrollment. This is not a “total cost of care model” that requires participants to manage to total cost of care targets, and as such can be combined with participation in ACOs or other APMs. It does not limit billing for most other clinical care but does take the place of certain care management billing codes.
Adjustments: Monthly payments will be adjusted for performance and health equity.
Respite Services: Participants will be reimbursed under the model for respite services for beneficiaries with a caregiver and moderate to severe dementia, up to a $2,500 annual cap for at home, adult day health or facility-based care. Stakeholders are raising questions about interactions with pre-existing opportunities to bill for respite under state Medicaid programs, and CMMI has said that further guidance will be forthcoming.
Participation in the Model
Eligible Beneficiaries: The GUIDE model is a voluntary model for both providers and beneficiaries, who must affirmatively consent to be aligned to a provider participating in the model. To be eligible for GUIDE, beneficiaries:
- Must be enrolled in Traditional Medicare fee-for-service Parts A and B
- May be dual eligible and enrolled in Medicaid
- May not be enrolled in an MA plan, though MA plans may choose to align their approach with GUIDE
- Must have a dementia diagnosis (at any stage)
- Cannot reside in a long-term nursing home
- Cannot be enrolled in PACE or Hospice
Eligible Providers: Model participants can be either single provider organizations enrolled in the Medicare program, or multiple organizations or partnering providers working together to be able to meet all required services; non-Medicare-enrolled organizations, including community-based organizations (CBOs), may participate in partnership with Medicare-enrolled provider organizations.
Primary Billing Provider Requirements: The main applicant and billing provider must be a Medicare Part B-enrolled provider/supplier, excluding durable medical equipment (DME) and laboratory suppliers, who can bill for Medicare Physician Fee Schedule services and agree to meet the care delivery requirements of the model. The primary enrolled provider must include at least one “dementia proficient clinician” defined as able to bill E/M codes and at least one of the following:
- At least 25% of the clinician’s patient panel comprised of adults with any cognitive impairment, including dementia
- At least 25% of the clinician’s patient panel aged 65 years old or older
- Have a specialty designation of neurology, psychiatry, geriatrics, geriatric psychiatry, behavioral neurology or geriatric neurology
Additional requirements that can be met by a primary organization or partnering organization are as follows:
- Must have interdisciplinary team that includes a care navigator, and may include other team members
- Training and education for care team members and for beneficiaries and caregivers
- 24/7 support
- Respite services
The model will offer two tracks:
- New Programs: Must not be operating a comprehensive community-based model at the time of model announcement and will have a one-year pre-implementation period to establish their programs.
- Established Programs: Must have an interdisciplinary care team, use Certified Electronic Health Record Technology (EHR) and meet other care delivery requirements that CMS will specify in its RFA.
Considerations for Potential Providers
Although not exclusively long-term supports and services, serious illness or palliative care models, existing palliative care and other serious illness programs may qualify as established or new programs. Providers who do not have compliant electronic health records must partner with entities that do. This model will require collaboration among a number of existing providers and technology partners, particularly for new programs.
Considerations for States and Other Payers
While this model is for Traditional Medicare beneficiaries, other payers and states may want to consider how this model could amplify or scale models of care that serve and focus on this population, or how they may want to adopt models of care or payment that would amplify the impact of this model. This may be especially true for MA plans and for Medicaid programs considering incentivizing coordination for health plans and providers who serve dual-eligible Medicare-Medicaid individuals.
Next Steps and More Information
- CMS accepted optional letters of interest (LOIs) for the GUIDE model through September 15, 2023, and will release an RFA for the model in fall of 2023 (open for all qualifying applicants, including those who did and did not submit an LOI).
- For more information on the GUIDE Model, click here to view Manatt Health’s and CMS’s recent free webinar, Guiding an Improved Dementia Experience: A Deep Dive into CMS’s New GUIDE Model.
- Click here to access CMS’s recently updated GUIDE Model Frequently Asked Questions.
- The model will launch on July 1, 2024, and run for eight years. CMS will release an RFA in fall of 2023, and further details will be forthcoming.
Contact Edo Banach at ebanach@manatt.com for help with any aspect of this important new model.